A study predicts that by 2050, superbugs may cause the death of around 40 million individuals.
Deaths from drug-resistant infections may rise by 70% in the next 25 years globally.
A recent study has projected that by the year 2050, there could be a 70 percent increase in the number of lives lost worldwide due to infections that are resistant to the medications meant to cure them. This highlights the severity of the ongoing superbug crisis that we are facing. The study, published in the journal The Lancet, estimates that from 2025 to 2050, there could be over 39 million deaths attributed to antimicrobial resistance (AMR).
AMR occurs when bacteria and fungi develop the ability to resist the effects of medications used to treat them. The World Health Organization has labeled AMR as one of the top global public health threats, caused by the misuse and overuse of antimicrobial drugs in humans, animals, and plants. This can lead to the development of resistant pathogens.
The United Nations General Assembly is set to hold a high-level meeting on September 26th to discuss the potential catastrophic impacts of AMR. Lead author of the study, Dr. Chris Murray, director of the Institute for Health Metrics and Evaluation at the University of Washington, warns that the situation is only expected to worsen. He emphasizes the need for attention to be given to the development of new antibiotics and better use of existing ones.
The burden of AMR falls heavily on older adults, according to the study. The researchers, from various institutions, looked at 22 pathogens, 84 pathogen-drug combinations, and 11 infections in 204 countries and territories from 1990 to 2021. They found that while deaths from AMR decreased by over 50 percent in children under 5, they increased by over 80 percent in adults over 70. These trends are projected to continue.
Murray notes that they were surprised to see these patterns emerge. The decline in AMR deaths among children is mostly due to the success of vaccination, water and sanitation programs, and treatment programs. However, there has been a steady increase in deaths among older adults, who may be more vulnerable to severe infections as they age.
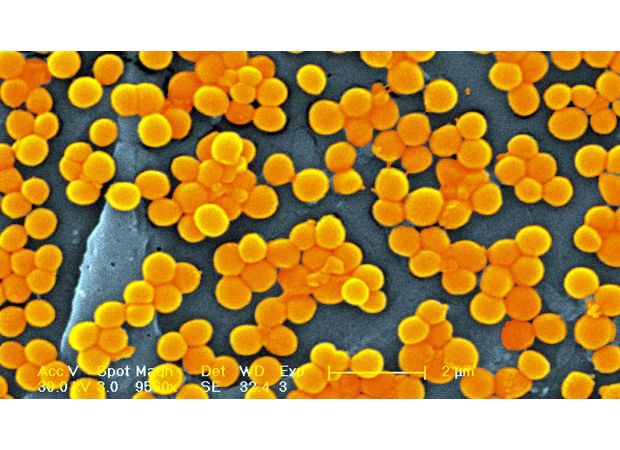
The study also looked at the pathogen-drug combinations that are causing the most burden among different age groups. The combination that saw the largest increase in attributable deaths was methicillin-resistant Staphylococcus aureus (MRSA). The number of deaths attributed to this combination almost doubled from 1990 to 2021.
Using statistical modeling, the researchers also made predictions for 2050 in three scenarios: if things continue as they are, if we develop more potent antibiotics, and if we improve access to quality healthcare and antibiotics. The results showed that without proper measures in place, deaths from AMR will continue to rise in the future. It is crucial to improve access to quality care, effective antibiotics, and other resources to reduce and treat infections.
According to a recent study published in The Lancet, the number of lives lost due to infections resistant to medication is predicted to rise by 70% by the year 2050. This paints a grim picture of the ongoing superbug crisis and highlights the burden it places on our world.
The study forecasts that from 2025 to 2050, more than 39 million deaths could be directly attributed to antimicrobial resistance (AMR). This means that the medications intended to combat these infections are no longer effective in treating them. AMR occurs when pathogens, such as bacteria and fungi, develop the ability to evade the drugs used to kill them.
The World Health Organization has labeled AMR as one of the top global public health and development threats. This is mainly due to the misuse and overuse of antimicrobial medications in humans, animals, and plants, which leads to the development of resistance in pathogens. In fact, the UN General Assembly is holding a meeting in September to discuss the potential catastrophic effects of AMR.
Dr. Chris Murray, the lead author of the study and director of the Institute for Health Metrics and Evaluation at the University of Washington, states that the prevalence of AMR is expected to worsen. He emphasizes the need for attention to be given to developing new antibiotics and implementing antibiotic stewardship to tackle this significant problem.
The burden of AMR falls heavily on older adults, as revealed by the study. Researchers estimated deaths and illnesses attributable to AMR versus those associated with it for various age groups and countries. They found that while deaths among children under 5 have decreased due to successful vaccination and treatment programs, deaths among adults 70 and older have increased by 80%. This is due to factors such as the aging population and the increased vulnerability of older adults to severe infections.
The pathogen-drug combination that caused the most burden among all age groups was methicillin-resistant Staphylococcus aureus, or MRSA. This combination, which is resistant to the antibiotic methicillin, has seen a significant increase in deaths from 57,200 in 1990 to 130,000 in 2021. Additionally, using statistical modeling, the researchers projected three scenarios for deaths and illnesses attributable to AMR by 2050. These include the current situation, the development of potent new antibiotics, and improved access to quality healthcare and antibiotics. The forecasts show a dire situation if measures are not taken to improve access to care and resources to reduce and treat infections.
In conclusion, the study highlights the urgent need to address the growing threat of AMR and implement effective measures to combat it. Without proper attention and action, the number of deaths and illnesses due to resistant infections will continue to rise and have catastrophic consequences for our world.






